
Common Pet Health Issues and How to Prevent Them
As pet parents, it’s important to keep our furry friends healthy and happy. While there are a variety of issues that can affect pets, some


As pet parents, it’s important to keep our furry friends healthy and happy. While there are a variety of issues that can affect pets, some

Allergies are e a common issue for pets, just as they are for humans. Recognizing the signs of allergies in your pet and knowing how

Fleas, ticks, and other pests can pose a serious threat to your pet’s health. These parasites can cause a range of health problems, from skin

As pet parents, it’s important to keep our furry friends healthy and happy. While there are a variety of issues that can affect pets, some
Understanding the importance of nutrition for your pet is crucial for their overall health and well-being. Providing your pet with a well-balanced diet can help

Most pet owners do everything they can to protect the well-being of their dogs and cats, but one thing they often neglect to check is

After being cooped up inside this winter, people and their pets are quick to race outside to hit the walking trails or lounge around the

by Dr. Jennifer Davis One year in a cat’s life is similar to five years in ours, so a lot can change in a year.

by Dr. Jennifer Davis One year in a dog’s life is similar to seven years in our life, so it’s important for dogs to get

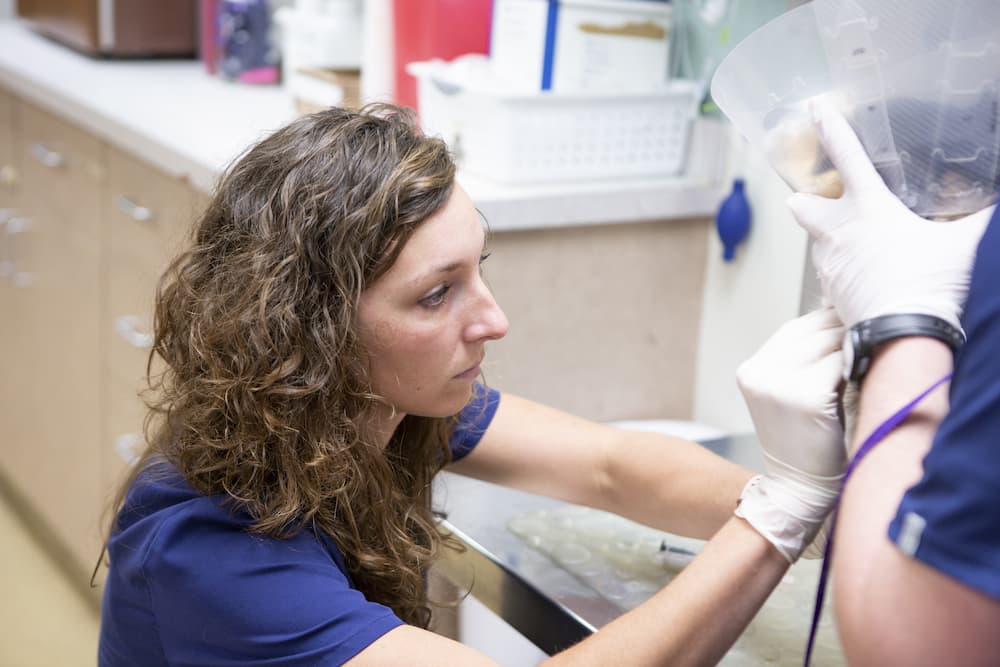
These friendly reptiles make wonderful pets, and when cared for properly, have a lifespan of 8-15 years. In captivity, bearded dragons are very social and